Prescriptions for accelerating translation: Q&A with Dr. Mustafa Sahin
TIDO had the pleasure of sitting down with Mustafa Sahin, MD, PhD, a neurologist at Boston Children’s and the director of the Translational Neuroscience Center, to talk about his motivations as a clinician-scientists, what he is doing to accelerate the translation of research to the clinic and how he successfully works with industry partners.
1. What drives you as a scientist? |
 What drives me as a scientist has changed over the course of my career. It was my fascination withexperimentation that got me first interested in biology. I took vials of fruit flies from my high-school to a radiation oncology department and tested effects of radiation on the mutation rate. Then, I came to the US to study biochemistry in college and was drawn to the mysteries of the brain. While my PhD and postdoctoral work continued on very fundamental questions about how neurons connected to each other, advances in genetics and neuroscience allowed me to bring rigorous basic science approaches to clinical questions. So more and more, my science is driven by a need to bring treatments to the patients I see in the clinic. Fortunately, this is no longer a long-term, aspirational goal, but something within reach in my career. |
2. What is unique about your research? |
| It is not unique to me at BCH, but designing experiments with the goal of accelerating our ability to treat patients is an important aspect of my research program. |
3. What unmet needs does your research aim to solve? |
| Treatments for neurodevelopmental disorders. Through the Human Neuron Core, we test already FDA approved compounds through a screening library on induced pluripotent stem cells (iPSCs) that have been differentiated into neurons. We also conduct phase II/III clinical trials for multiple neurogenetic disorders with novel compounds. We hope through these multiple initiatives, we will repurpose already existing drugs and identify novel treatments. |
4. What tools are you/BCH developing to better study neurological diseases? |
One of the things we realized about 5 years ago, when the first clinical trials in neurodevelopmental disorders were starting to come online, was the fact that we did not have a well-organized infrastructure in neurosciences for bringing therapies from the lab to the clinic in an efficient manner. Every investigator had to develop their own team to overcome commonly faced obstacles. So, we developed the Translational Neuroscience Center (TNC) from the bottom up as an integrated facilitator for enhancing translational studies in brain and nervous system disorders, encompassing neurodevelopmental and neuropsychiatric disorders, neuromuscular diseases and pain. As a part of the TNC, we now have platforms to help investigators all the way from target discovery to Phase II clinical trials.
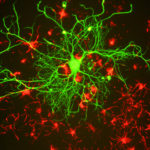 For example, our Human Neuron Core can facilitate target identification, validation and drug screens. We have an Electrophysiology Core for performing parallel EEG-based studies in animal models and patients. Our Regulatory Core can help investigators with IRB, IND, and project management. Our Human Neurobehavioral Core Services can provide expert and detailed phenotyping for cognitive/behavioral outcome measures. With these enhancements, we are now in a position to take the lead on performing clinical trials in children with nervous systems disorders. |
5. What is your favorite model in neuroscience/tool to model neurological disease? |
| I am not a scientist who has a favorite model or tool. We have let the disease (in our case Tuberous Sclerosis – TSC) guide us from model to model, tool to tool as necessary. Animal models, in particular genetically engineered mice, have been the mainstay of our research. However, it has some significant drawbacks. For that reason, we have increasingly turned to human neurons in a dish as an additional new model. Last year, we published two papers where we used a combination of mouse experiments and human neurons. I think this combinatorial approach will be even more powerful than either one alone. |
6. How can studying pediatric neurological diseases inform the study of adult diseases? |
 First, many of the cell biological processes we study in pediatric neurological diseases such as TSC have important roles in adult neurodegenerative diseases as well. These include autophagy, mitochondrial dynamics, endoplasmic reticulum stress, oxidative stress, synapse pruning, etc. Second, given the early plasticity of the brain, the therapeutic window for treatments is likely to be in infancy-childhood and allow us to alter the disease progression. The same concept is likely to apply to at least some adult neurological diseases, too. Finally, due to the fact that pediatric diseases affect developing brain/neurons, they may be easier to model in animal models (that do not live for decades) or in cell culture. So, investigating and screening for compounds in pediatric neurological disease models may give us insights and therapies for some of the adultdisorders as well. |
7. How can academia better de-risk translation of targets or candidate drugs for industry development? |
| Industry is in search of drugs which have reasonably large effect sizes and are reproducible in one or more models. The incentives in academia (publishing high profile manuscripts rapidly) often do not align with the ultimate goals of industry. Many academic publications use a drug only in one concentration, do not demonstrate target engagement in the target organ nor provide any pharmacokinetic information. Both through our Translational Research Program (TRP) grants and the activities of the Translational Neuroscience Center (TNC), we have been working towards addressing this gap. We have a drug-discovery mini-course offered by the Translational Neuroscience Center that focuses on neuroPK for academic investigators. In every experiment performed in the TNC Neurophysiology Core, we urge the investigators to measure brain PK and target engagement as much as is feasible. We hope these efforts will not only de-risk targets/drugs for industry but will also make the studies of BCH investigators more reproducible with higher translational impact. |
8. You have collaborated with large and small biotech companies on several projects. What is the most important element for a successful industry-academia collaboration? What has each side brought to the table, and how has each benefited from collaboration? |
| Academic-Industry partnerships are key in rare disorder research where much of the early preclinical work is already being done at Boston Children’s. We are also fortunate to care for patients with rare diseases from across the world that can be enrolled in research. Industry has been helpful in coordinating the large Phase III clinical trials amongst multiple hospitals nationally and internationally. We have also done a number of projects with companies in our Human Neuron Core. In all of these cases, involving the Technology & Innovation Development Office and the Clinical Trials Business Office has been essential for success, allowing for clear deliverables and streamlining communication with sponsors. The most successful collaborations have been those in which there are scientists championing for the project on both sides (BCH and industry). Often, we bring models (animal or cell models that we have developed at BCH) and the company brings novel compounds that we could not have access to otherwise. Together, we are able to probe biological problems in a way we cannot do in either setting alone. |
